Bariatric surgery is considered an effective treatment for obesity in individuals who have not had long-term success with other measures for weight loss.
To be considered for weight loss surgery, each patient must view our educational seminar and complete a new patient health history form. You can complete these steps by clicking the “Get Started” button below. If you encounter any technical issues, please call our office at 573-248-5407 for assistance.
Get Started Contact Us
Bariatric Surgery at Hannibal Regional includes the procedures below: Gastric Bypass (RYGB), Sleeve Gastrectomy (LSG), Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S), and Biliopancreatic Diversion with Duodenal Switch (BPD/DS). See below for more details and learn more at the links in the sidebar.
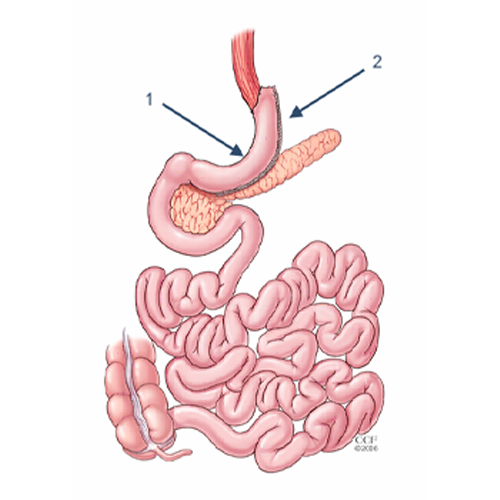
The Gastric Bypass Procedure
The Roux-en-Y Gastric Bypass – often called gastric bypass – is considered the ‘gold standard’ of weight loss surgery.
There are two components to the procedure. First, a small stomach pouch, approximately one ounce or 30 milliliters in volume, is created by dividing the top of the stomach from the rest of the stomach. Next, the first portion of the small intestine is divided, and the bottom end of the divided small intestine is brought up and connected to the newly created small stomach pouch. The procedure is completed by connecting the top portion of the divided small intestine to the small intestine further down so that the stomach acids and digestive enzymes from the bypassed stomach and first portion of small intestine will eventually mix with the food.
The gastric bypass works by several mechanisms. First, similar to most bariatric procedures, the newly created stomach pouch is considerably smaller and facilitates significantly smaller meals, which translates into less calories consumed. Additionally, because there is less digestion of food by the smaller stomach pouch, and there is a segment of small intestine that would normally absorb calories as well as nutrients that no longer has food going through it, there is probably to some degree less absorption of calories and nutrients.
Most importantly, the rerouting of the food stream produces changes in gut hormones that promote satiety, suppress hunger, and reverse one of the primary mechanisms by which obesity induces type 2 diabetes.
Advantages of Gastric Bypass
- Produces significant long-term weight loss (60 to 80 percent excess weight loss)
- Restricts the amount of food that can be consumed May lead to conditions that increase energy expenditure
- Produces favorable changes in gut hormones that reduce appetite and enhance satiety
- Typical maintenance of >50% excess weight loss
- Involves a relatively short hospital stay of approximately 1-2 days
Disadvantages of Gastric Bypass
- Is technically a more complex operation than the LSG and potentially could result in greater complication rates
- Can lead to long-term vitamin/mineral deficiencies particularly deficits in vitamin B12, iron, calcium, and folate
- Requires adherence to dietary recommendations, life-long vitamin/mineral supplementation, and follow-up compliance
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy – often called the sleeve – is performed by removing approximately 80 percent of the stomach. The remaining stomach is a tubular pouch that resembles a banana.
The Procedure
This procedure works by several mechanisms. First, the new stomach pouch holds a considerably smaller volume than the normal stomach and helps to significantly reduce the amount of food (and thus calories) that can be consumed. The greater impact, however, seems to be the effect the surgery has on gut hormones that impact a number of factors including hunger, satiety, and blood sugar control.
Short term studies show that the sleeve is as effective as the roux-en-Y gastric bypass in terms of weight loss and improvement or remission of diabetes. There is also evidence that suggests the sleeve, similar to the gastric bypass, is effective in improving type 2 diabetes independent of the weight loss. The rates of complications related with the sleeve gastrectomy are less than gastric bypass. There is no marginal ulcer formation, internal hernia, and less likely to have stricture and vitamin deficiency.
Advantages of the Sleeve Gastrectomy Procedure
- Restricts the amount of food the stomach can hold
- Induces rapid and significant weight loss that comparative studies find similar to that of the Roux-en-Y gastric bypass. Weight loss of >50% for 3-5+ year data, and weight loss comparable to that of the bypass with maintenance of >50%
- No bypass or re-routing of the food stream as in the gastric bypass
- Involves a relatively short hospital stay of approximately 1-2 days
- Causes favorable changes in gut hormones that suppress hunger, reduce appetite and improve satiety
Disadvantages of the Sleeve Gastrectomy Procedure
- Is a non-reversible procedure
- Has the potential for long-term vitamin deficiencies
- If complication of leak occurs, this is slower to heal compared to gastric bypass
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
The Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy, referred to as the SADI-S is the most recent procedure to be endorsed by the American Society for Metabolic and Bariatric Surgery. While similar to the BPD-DS, the SADI-S is simpler and takes less time to perform as there is only one surgical bowel connection.
The Procedure
- The operation starts the same way as the sleeve gastrectomy, making a smaller tube-shaped stomach.
- The first part of the small intestine is divided just after the stomach.
- A loop of intestine is measured several feet from its end and is then connected to the stomach. This is the only intestinal connection performed in this procedure.
How it Works
When the patient eats, food goes through the pouch and directly into the latter portion of the small intestine. The food then mixes with digestive juices from the first part of the small intestine. This allows enough absorption of vitamins and minerals to maintain healthy levels of nutrition. This surgery offers good weight loss along with less hunger, more fullness, blood sugar control and diabetes improvement.
Advantages
- Highly effective for long-term weight loss and remission of type 2 diabetes
- Simpler and faster to perform (one intestinal connection) than gastric bypass or BPD-DS
- Excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss
Disadvantages
- Vitamins and minerals are not absorbed as well as in the sleeve gastrectomy or gastric band
- Newer operation with only short-term outcome data
- Potential to worsen or develop new-onset reflux
- Risk of looser and more frequent bowel movements
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
The Biliopancreatic Diversion with Duodenal Switch, abbreviated BPD-DS, begins with creation of a tube-shaped stomach pouch similar to the sleeve gastrectomy. It resembles the gastric bypass, where more of the small intestine is not used.
The Procedure
- Following creation of the sleeve-like stomach, the first portion of the small intestine is separated from the stomach.
- A part of the small intestine is then brought up and connected to the outlet of the newly created stomach, so that when the patient eats, the food goes through the sleeve pouch and into the latter part of the small intestine.
How it Works
The smaller stomach, shaped like a banana, allows patients to eat less food. The food stream bypasses roughly 75% of the small intestine, the most of any commonly performed approved procedures. This results in a significant decrease in the absorption of calories and nutrients. Patients must take vitamins and mineral supplements after surgery. Even more than gastric bypass and sleeve gastrectomy, the BPD-DS affects intestinal hormones in a manner that reduces hunger, increases fullness and improves blood sugar control. The BPD-DS is considered to be the most effective approved metabolic operation for the treatment of type 2 diabetes.
Advantages
- Among the best results for improving obesity
- Affects bowel hormones to cause less hunger and more fullness after eating
- It is the most effective procedure for treatment of type 2 diabetes
Disadvantages
- Has slightly higher complication rates than other procedures
- Highest malabsorption and greater possibility of vitamins and micro-nutrient deficiencies
- Reflux and heart burn can develop or get worse
- Risk of looser and more frequent bowel movements
- More complex surgery requiring more operative time